I haven’t been very active blogging lately, so in true blogging style, here is a filler-post rounding up my year!
This year I started to get back to writing after a bit of a thesis-writing hiatus. I’ve had a bit more time to think about the sort of direction I wanted to take my writing in. The biggest change I’ve made is deciding to put my own name to my writing on here, linking together my professional/academic work and my personal experiences. I’ve been asked if I found this “exposing” – the reality is it’s made very little difference. Using my own name has facilitated making connections with other people, both other professionals and others who have had similar experiences to my own. I haven’t experienced any negative consequences, and though I can’t rule out that this could still happen in the future, I feel prepared to defend my own openness. This year I began supervising an assistant psychologist who disclosed their own lived experience and asked my advice on managing this disclosure, and I felt well-placed to give them advice on this.
This blog started as a bit of a catch-all for my writing on topics I found interesting. I’ve made it a bit more focused now, so it predominantly covers professional issues in healthcare, mental/physical health, disabilities/rehabilitation and sexuality/gender issues. Cutting away the more “frivolous” topics (less fashion and pages of photos) has led to a decline in my site hits, but I think the content is better quality (though less widely searched!). I’ve been so busy at work that I’ve been online a lot less, so I feel a bit less involved in the community and might now need to work to become a bit more visible.
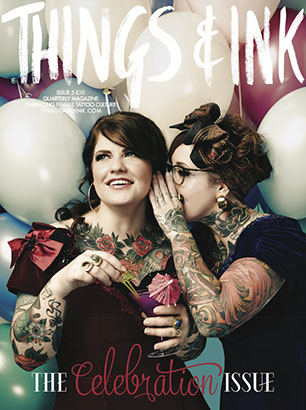
This year I’ve also written a few pieces for some other sources – the online blog for Things & Ink Magazine, Discursive of Tunbridge Wells Blog and more recently the Guardian Healthcare Network. Writing for other sources encourages me to be more disciplined and also expands the reach of my work. Now that I’ve qualified and given some of the political changes recently I feel even more strongly about public engagement and bringing greater awareness to “hidden” issues.
After a year in my first qualified post I made a change, moving out of neurorehabilitation and expanding into health psychology more generally. I now work with people with HIV, Medically Unexplained Symptoms and long-term neurological conditions, as well as brain injury. I love working in this exciting mental health/physical health borderland, we’re trying to bring mind and body together. I’m learning so much. I’ve also become more involved in my local DCP and hope to continue this. Like many, I often feel frustration and apathy towards my professional body and about my place within the NHS. It’s easy to feel powerless and resentful, and it can be hard to find the time (and sometimes money!) to really be a part of things. But as they say, be the change you hope to see in the world, and all. I am finding my own way to be involved, connect with others and create something.
A few goals for the new year:
- Blog more often! Finish all my half-written posts
- Collaborate! I have so many people I want to get projects together with, time to turn ideas into action
- Pitch more articles to other sources. I’d like to write some pieces for more mainstream places, even if less academic these places get the message out successfully
- Be more active in my professional body and activism, locally and wider afield
- Spruce the blog up a bit, maybe even get one of those paid accounts so I can avoid getting awful diet ads on the thing
A few of the posts I’ve not entirely finished but will emerge soon are:
- Incorporating sex-positivity into healthcare
- Disillusionment with the trend for “mindfulness” (or how I tried and failed to be more mindful)
- Meaningful occupation and why just any old job isn’t necessarily good for well-being
- Narratives about (dis)ability and how this limits rehabilitation potential
- Community psychology/social justice approaches to rehabilitation (beyond the rehab room!)
- Planning a feminist wedding and muscle-related body image (or why I love weight-lifting even though it doesn’t make me look “pretty”). If anyone wants to get involved in any of the above let me know and they may yet see the light of day!
Great thanks to everyone who has supported me over the last year, I hope you’ve all had a lovely Xmas and wish you all the best for the new year.
 As a newly appointed HIV psychologist, I’ve been taking some time to better inform myself. I’ve been reading NAM’s
As a newly appointed HIV psychologist, I’ve been taking some time to better inform myself. I’ve been reading NAM’s